
-
How Long Does It Take To Recover From Minimally Invasive Gynecologic Surgery?
posted: Sep. 21, 2023.

-
When Should a Girl See a Gynecologist for the First Time?
posted: Sep. 19, 2023.

-
What Are the Stages of Menopause?
posted: Sep. 16, 2023.

-
What Are Causes of Infertility in Women?
posted: Sep. 14, 2023.

-
Benefits of Having an OBGYN
posted: Sep. 12, 2023.

-
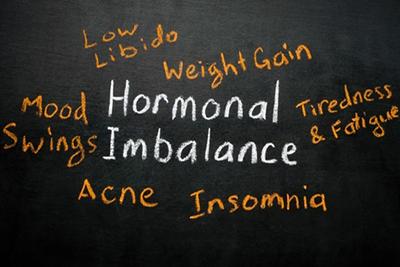
What Are the Signs and Symptoms of Hormonal Imbalance?
posted: Sep. 11, 2023.
-
What To Know About Irregular Bleeding
posted: Sep. 01, 2023.

-
What You Can Expect During Menopause
posted: Aug. 23, 2023.

-
Menopause: How Will I Know?
posted: Aug. 14, 2023.

-
When To Visit an OBGYN
posted: Aug. 01, 2023.

-
Managing Menopause: Tips for a Smooth Transition
posted: Jul. 19, 2023.

-
Common Gynecological Conditions: Causes, Symptoms, and Treatment
posted: Jul. 05, 2023.

-
When Should You See an OBGYN?
posted: Jun. 23, 2023.

-
Common Causes of Painful Periods
posted: Jun. 05, 2023.

-
Common Gynecological Conditions and How to Treat Them
posted: May 22, 2023.

-
Questions to Ask Your OB/GYN About Birth Control
posted: May 09, 2023.

Our Location
Find us on the map
Hours of Operation
Our Regular Schedule
Primary Location
Monday:
9:00 am-5:00 pm
Tuesday:
9:00 am-5:00 pm
Wednesday:
9:00 am-5:00 pm
Thursday:
9:00 am-5:00 pm
Friday:
9:00 am-3:00 pm
Saturday:
Closed
Sunday:
Closed